Food allergies: 5 myths explained
Food allergies seem to be on the rise, but misconceptions abound, often getting in the way of a condition being properly diagnosed and treated. According to recent research, up to 35 percent of people misdiagnose themselves (or their kids) with a food intolerance or allergy. They then try to manage it themselves, rather than seeking proper medical advice. So it’s time to set the record straight on five of the most popular misconceptions.

1. I have symptoms after food so it must be an allergy
Not necessarily. Adverse reactions to a food can occur for a variety of reasons. They all fall within the umbrella term “food hypersensitivity”. This includes reactions that involve the immune system, known as a “food allergy”. But it also includes a range of others that don’t involve the immune system – commonly called a “food intolerance”.
Allergic reactions that involve the antibody immunoglobulin E are often referred to as IgE-mediated food allergies. According to the Centre for Food and Allergy Research, Australia has the highest prevalence of IgE-mediated food allergy in the world, with 10 percent of infants having a proven food allergy. IgE-mediated food allergies cause symptoms that range from mild (such as itchy eyes) to severe, including anaphylaxis. This is a serious, swift allergic reaction that can cause severe throat or tongue swelling, difficulty breathing, low blood pressure and even death. These symptoms usually occur rapidly after eating the food in question and when severe, require immediate medical attention.
Other reactions that involve the immune system (known as non-IgE mediated allergy) may cause symptoms that are either immediate or slower in onset and are more chronic in nature. These can include red, itchy skin, heartburn or loose stools. Some of these may be similar to symptoms caused by food intolerances. While totally excluding the trigger food is usually required in IgE food allergy, restricting it may be sufficient in other forms of hypersensitivity. However, this will depend on the underlying cause.

2. I can just go online and get an allergy test
A trip to the chemist or a browse online for a diagnosis is likely to provide you with a large bill and a long list of foods that are apparently causing your symptoms. Many of the tests offered are not evidence-based for food allergy or food intolerance. These can lead to unwarranted self-imposed dietary restrictions. This not only increases the risk of nutritional deficiency, it can cause anxiety and ultimately affect your quality of life.
The only evidence-based allergy testing currently available is for IgE (immediate reaction) allergy. These are skin-prick tests and specific IgE blood tests. However, even if IgE testing is offered, the results still require careful interpretation. A positive test doesn’t necessarily mean you have an allergy. An “oral food challenge”, where precise and increasing doses of the suspect food are given, is considered the best method of diagnosis for food allergies. However, these must be performed with medical supervision.
Diagnosis starts with a thorough, allergy-focused history that will point towards appropriate testing if required. This needs to be undertaken by a medical professional with experience in allergy. So, if you’re concerned about your symptoms, talk to your GP.

3. I need to avoid lots of foods to help control my eczema
This is unlikely. Food doesn’t cause eczema. There are also many environmental triggers implicated in eczema flare-ups. This makes it difficult to ascertain if cutting out specific foods is actually helping your symptoms. You don’t need to look far to find books and online resources that suggest a variety of implicated foods. But for most people, appropriate medical treatment is the key to controlling the condition.
That said, some people with atopic eczema may need to avoid certain foods due to fast onset and potentially severe IgE food allergy. Additionally, excluding specific foods may be beneficial for some and may involve non-IgE food allergy. However, this needs careful assessment. So if you feel your current treatment for eczema isn’t keeping it under control, speak to your doctor before making any dietary changes.
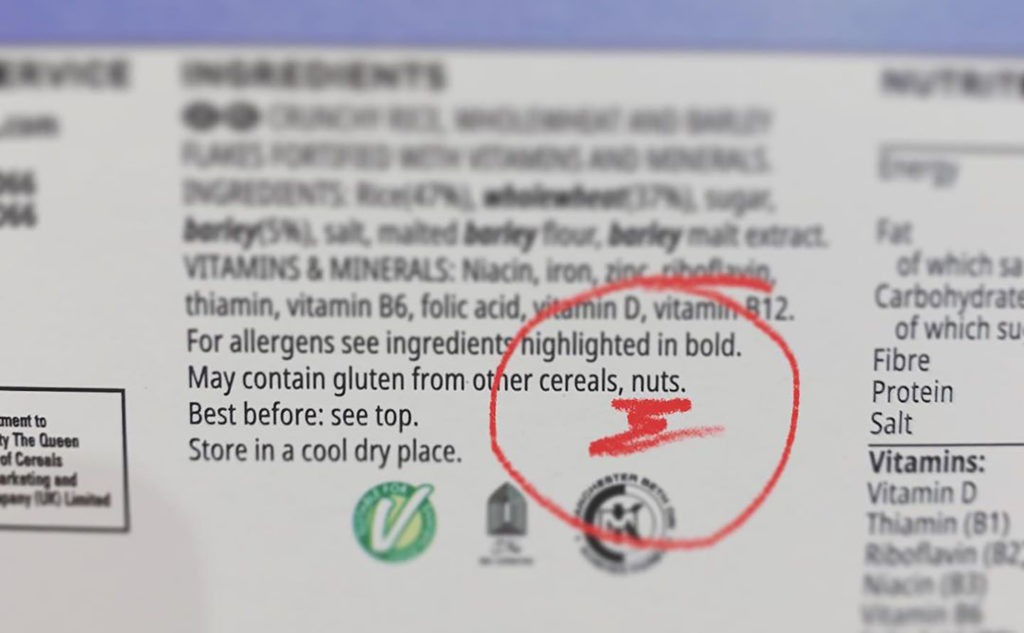
4. “May contain” warnings only protect manufacturers
Food labelling rules in Australia state that the nine most common allergens (peanut, tree nuts, milk, egg, fish, shellfish, wheat, sesame and soy) must be declared on packaging. In February this year, the Food Standards Australia New Zealand (FSANZ) Code was amended to introduce new requirements for the labelling of allergens in food sold in Australia. These requirements include that allergen information must be declared in a specific format and location on food labels, using simple, plain English terms in bold font.
However, the changes to the code provide no guidance for the use of “may contain” statements. These are voluntary statements made by food businesses and are not currently regulated by the code. And while food manufacturers must comply with allergen declaration requirements, “may contain” statements may not help a food manufacturer if the food is found to contain the allergen in question and there’s no allergen declaration on the label.
The safest approach for many people with food allergies is to avoid all products with these warnings. But how this is managed is down to personal choice. Understanding what is and isn’t required on food labelling is essential to making a fully informed decision about managing what you eat. You can find more information on the FSANZ website.

5. You just need to avoid the trigger food if you’re allergic
Many people following restricted diets would disagree. Not only is there a potential nutritional risk, excluding certain foods requires careful planning and constant vigilance. For those with fast-onset IgE allergy in particular, where accidental exposure to the trigger food may cause severe symptoms, this can result in considerable anxiety.
In fact, there’s evidence that having potentially severe food allergy has a detrimental effect on quality of life in terms of health. So proper advice and appropriate management is a must. With an abundance of information available, thanks mainly to online sources, it’s more important than ever to make sure you use credible, reliable sources. You should also seek proper medical advice if you’re concerned about food-related symptoms.
This article was written by Marian Cunningham, lecturer in Human Nutrition and Dietetics, Glasgow Caledonian University, Scotland; and was originally published by The Conversation. The article has been edited for style and clarity.









